Anterior Knee Pain
What is Chondromalacia Patellae?
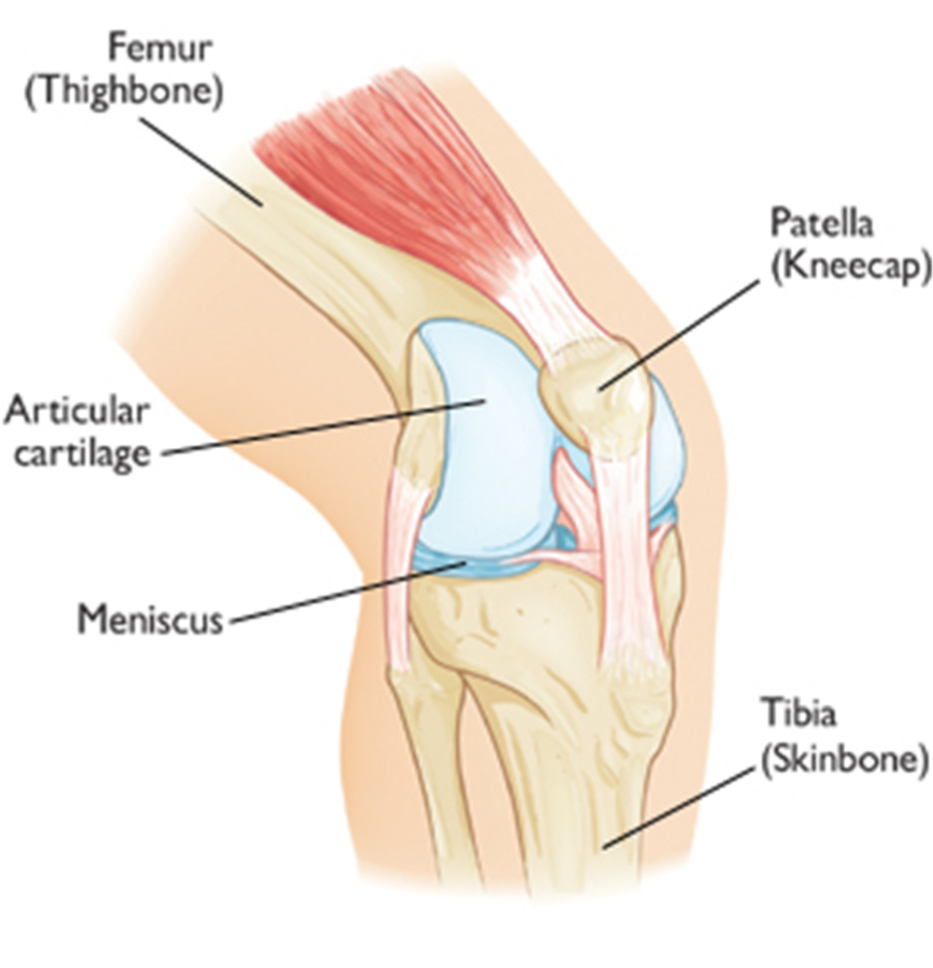
Chondromalacia,technically termed Chondromalacia Patellae, is the most common cause of chronic knee pain. The condition develops due to softening of the cartilage beneath the kneecap (patella), resulting in small areas of breakdown and pain around the knee. Instead of gliding smoothly over the knee, the knee cap rubs against the thigh bone (the femur) when the knee moves. The changes can range from mild to complete erosion of the cartilage. This process may sometimes be referred to as patellofemoral syndrome.
What causes chondromalacia patellae?
The patella is normally pulled over the end of the femur in a straight line by the quadriceps (thigh) muscle. Patients with Chondromalacia patellae frequently have abnormal patellar ‘tracking’ toward the outer side of the femur. This slightly off-kilter pathway allows the under-surface of the patella to grate along the femur causing chronic inflammation and pain.
This may occur because:
- the kneecap is in an abnormal position (also called poor alignment of the patellofemoral joint)
- there is tightness or weakness of the muscles on the front and back of your thigh
- you are doing too much activity that places extra stress on the kneecap (such as running, jumping or
twisting) - you have flat feet
Certain individuals are predisposed to develop Chondromalacia patellae: females, knock-kneed or flat-footed runners, or those with an unusually shaped patella under-surface. However it can affect any member of the population, and may present itself due to one of the following reasons:
Adolescent knee pain
- Usually at the beginning of a growth spurt, either due to overuse or no apparent reason.
- Can continue throughout childhood and become a chronic condition.
- Often affects the ability to compete in sports.
Direct trauma (dashboard knee)
- Knee pain continues after the trauma has healed and persists affecting the quality of life.
- This can occur with or without an associated fracture.
Indirect trauma (knee ligament injury)
- This is a chronic case where the pain continues, despite the healing of the ligaments of the knee.
Athletics
- This is the most common condition in sports.
- Often occurs after a change in training patterns, following an injury or for no apparent reasons.
Overuse
- The common factors being a severe change in activity which usually involves running, cycling or any
situation that requires a greater amount of walking or stair climbing.
What symptoms should I look out for?
- Dull, aching pain behind the kneecap (patella), worsening with activity
- A grating or grinding sensation when the knee is bent
- Giving way with a catching feeling
- Giving way while running
- Tenderness around the patella area is occasionally present.
How is it diagnosed?
Your doctor will take a complete medical history and perform a physical examination to help determine the cause of the pain. Make sure you inform your doctor about any sports participation or training you are involved in, and which activities aggravate your knee pain. The physical examination will include a check of the alignment of your lower leg, kneecap, and quadriceps, and will also incorporate an assessment of your hip rotation, the range of motion of knees and hips. The underside of your kneecap will be checked for signs of tenderness. Part of the examination may involve you being asked to perform certain movements to assess your knee’s strength, mobility and alignment, such as standing, walking, jumping, squatting, sitting, and lying down.
The surgeon may also order x-rays, MRI or CT scans to rule out any damage to the structure of the knee and its connective tissues.
What are the treatment options?
The primary goal for treatment and rehabilitation of chondromalacia patellae is to create a straighter pathway of the patella to follow during knee movement. Temporarily resting the knee and avoiding activities that cause knee pain, taking non-steroidal anti-inflammatory medications (NSAIDs) such as ibuprofen, naproxen or aspirin, may initially help to relieve pain. If you are overweight, losing weight will help to reduce pressure on your knee.
Following the RICE technique is beneficial:
- Rest – avoid overuse of the painful knee, possibly switching to a non-weight bearing activity such as swimming,
- Ice – applying cold packs several times a day can assist in reducing any swelling,
- Compression – a simple knee bandage or knee support,
- Elevation – raising the knee above the level of the heart can assist in reducing swelling.
Physiotherapy
After resting the knee until the pain and swelling go down, you may need reconditioning to regain full range of motion, strength, power, endurance, speed, agility, and coordination. Your physiotherapist may design an exercise program to regain the flexibility and strength of thigh muscles, or recommend cross-training exercises that emphasise stretching the lower extremities. Your doctor will tell you when you may gradually resume running and other activities.
Bracing
Taping the knee, or using a brace, can help in some cases, particularly during sports activities.
Orthotics
Special shoe inserts may help to relieve pain and realign the lower leg.
Do I need surgery?
Sometimes chondromalacia patellae is not cured by conservative therapy, and it may be determined that surgery is needed.
Surgical options include:
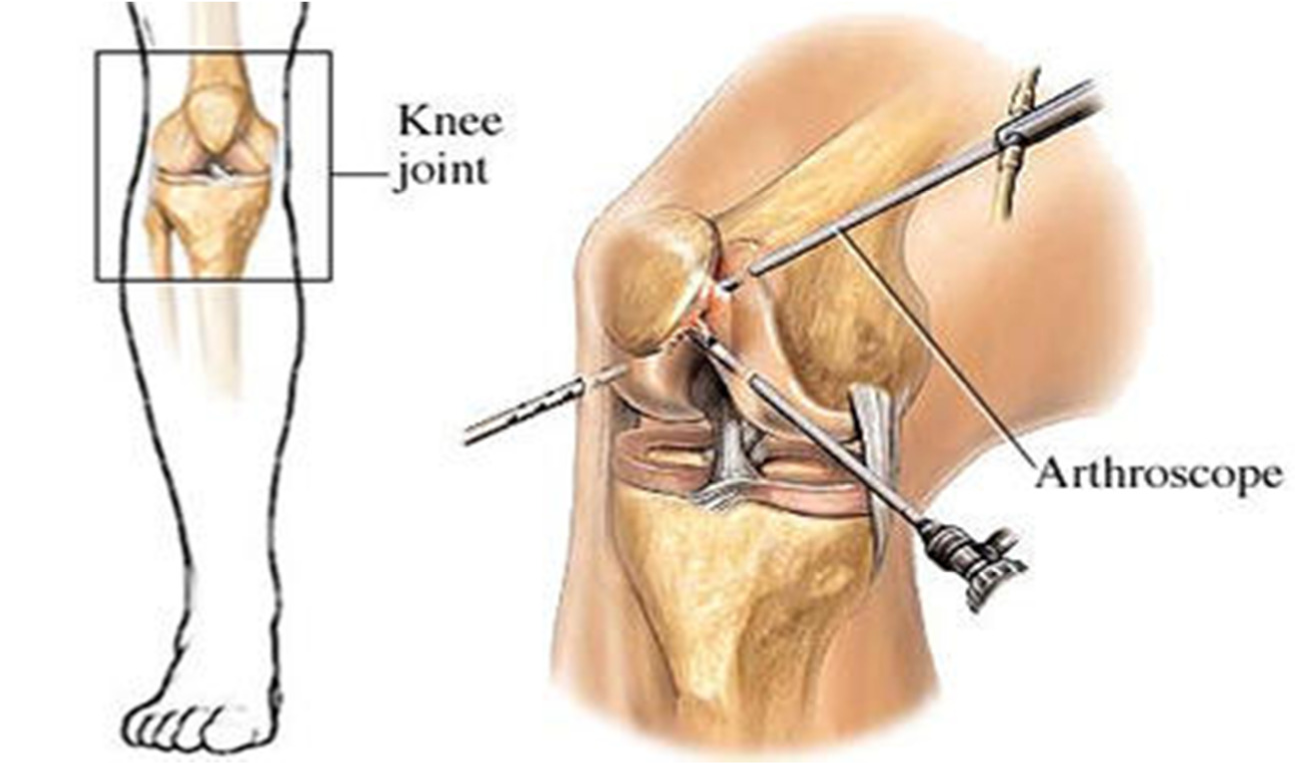
- Arthroscopy – The surgeon will make a small incision in the knee to allow a camera to be inserted. This camera is no wider than a pencil and allows the surgeon to see the structures of the knee and any damage that is present.
- Realignment – The surgeon uses a slightly larger incision to open the knee structure, and realigns the kneecap using a procedure known as a lateral release. This involves cutting the tight lateral ligaments to allow for normal position and tracking of the patella. If this is not sufficient to correct the misalignment, there is more extensive surgery that can be performed.
How important is rehabilitation in the treatment of chondromalacia patellae?
Stretching and strengthening the quadriceps and hamstring muscle groups is critical for an effective and lasting rehabilitation of chondromalacia patellae. A physiotherapist will see you after your surgery and discuss a plan for your rehabilitation. It would be expected that walking could begin immediately. However physiotherapy sessions could continue for several months.
Under optimal circumstances, the patient should have a rapid recovery and return at full functional level.
What can I do to look after my knee?
To protect your knee from further damage in the future, there are some things that you can do, or changes you can make to your activities, such as:
- Wear shoes appropriate to your activities, and consider orthotics if necessary
- Warm up with stretching exercises before physical activity
- Stop or reduce any activity that hurts your knees
- Avoid running straight down hills, walk instead
- Bicycle or swim instead of running
Maintaining a regular exercise or physiotherapy program focussing on strength and stability will be of benefit.
The patient information sheets are intended to provide general information only and are not a substitute for medical advice about your particular condition.